Though monkeypox cases continue to rise in the region, the county has yet to open vaccine clinics for the disease.
Supply of the monkeypox vaccine JYNNEOS remains “limited,” county spokesperson Ryan Hudson tells ARLnow, and Arlington is coordinating with the Virginia Department of Health to obtain and administer doses.
However, at this moment, there are no planned vaccine appointments or clinics to administer those doses in Arlington to those who are at higher risk and might have been exposed in the last 14 days.
“VDH is still working to expand vaccine access for Virginians who are at higher risk of being exposed to monkeypox and meet CDC criteria,” Hudson wrote ARLnow in an email. “Information about who will be eligible and how they get vaccinated will be provided when it becomes available both on the VDH site and County site.”
This is in contrast to D.C., which made limited, pre-registered monkeypox vaccine appointments available late last month.
While monkeypox cases are rising in Virginia, they remain relatively low compared to the District which has the highest rate of monkeypox cases per capita in the country.
As of this morning (Wednesday), the Virginia Department of Health is reporting that there are 56 cases of monkeypox in the Commonwealth. Three-quarters of those cases, 42, are in the Northern Region, which includes Arlington.
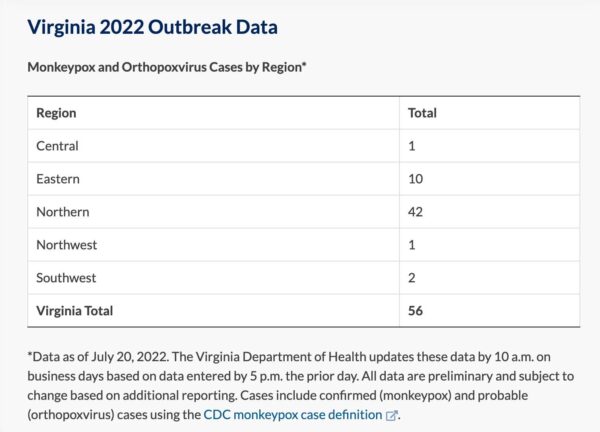
This is a relatively rapid rise from only a few weeks ago when, in late June, VDH announced there were only 8 cases in the entire Commonwealth. The first case in Northern Virginia was detected back in late May.
County Manager Mark Schwartz spoke briefly about monkeypox at the County Board meeting yesterday afternoon.
“Our Public Health Division is coordinating with the Virginia Department of Health and local health care providers to test for potential cases and to provide guidance on isolation and treatment,” Schwartz said. “We are reaching out also to and monitoring all contacts of potential cases.”
He also noted that the vaccine supply is “pretty limited” and “only being offered to residents who are at high risk of getting monkeypox and have likely been exposed in the last 14 days.”
Monkeypox can spread through direct contact with infectious rashes, scabs, body fluids, or through “respiratory secretions,” according to the CDC. This includes having “prolonged, face-to-face contact” or “intimate physical contact, such as kissing, cuddling, or sex” with someone who is infected.
The virus can spread to and make anyone sick, though the highest risk groups at the moment are men who have had sex with men and with multiple partners over the last several weeks, sex workers, transgender women and nonbinary persons who have sex with men, and people who work in places where sex occurs like saunas and bathhouses.
The CDC and VDH define “higher risk” as those who are in these groups and might have been exposed over the last 14 days.
Health agencies have struggled with messaging, in that the virus is impacting the male gay community more at this moment but agencies do not want to further stigmatize an already marginalized group.
Monkeypox causes rashing and potentially other symptoms over a course of several weeks. The West African type that’s making its way around the globe is “rarely fatal,” says the CDC website, though “symptoms can be extremely painful, and people might have permanent scarring resulting from the rash.”
If one is already infected with monkeypox, health officials note, the vaccine is not an effective treatment.
“If someone suspects they have a monkeypox infection, they should contact a healthcare provider,” writes Hudson.

