 Health Matters is a biweekly opinion column. The views expressed are solely the author’s.
Health Matters is a biweekly opinion column. The views expressed are solely the author’s.
Arlington started its vaccination efforts with healthcare workers days after the COVID vaccine was granted Emergency Use Authorization from the FDA last December.
Despite a somewhat turbulent rollout (concerns about being too slow, vaccination sites abruptly canceling appointments and line-jumping opportunists), vaccinations in Arlington are steadily rising. As a state, Virginia ranks #12 in the country with 69% of distributed vaccines administered.
As of this writing, 15,410 Arlingtonians have been vaccinated, with 2,409 being fully vaccinated. Does that mean everybody with vaccinations can finally ditch their masks? As liberating as disposing of facemasks would be, the short answer is: not yet. In fact, we shouldn’t really change much of our social distancing habits that we have honed over the year. I know, not another doctor trying to kill the feel-good buzz of a modern miracle–but hear me out. Here are 5 good reasons to keep your masks on after vaccination.
- You might still infect others.
It is unclear whether people who are vaccinated can get asymptomatic infections and spread it to those without the vaccine. Studies are being done in real-time to determine transmissibility of vaccinated, infected people.
- “Herd Immunity” takes time–and it’s not guaranteed
An estimated 60-70% of the population needs to be vaccinated before “herd immunity” could happen. Arlington currently stands at around 6.5% receiving the first vaccination, so it will take months to get near the 60-70% goal. Wearing masks will continue to help stop the spread while we get closer to that goal.
- COVID variants have been identified
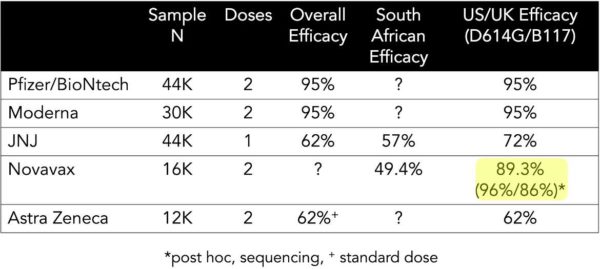
Studies on the variants from the UK, South Africa and Brazil are happening in real-time, and initial reports from the newer vaccines show less effectiveness against the variants.
Since the variants are so new, there is no published data for Pfizer or Moderna vaccines’ effectiveness against the variants. The mutations are believed to be more infectious/transmissable, further fueling anxiety and confusion. Until we get more data on the variants, wearing masks is still important to prevent spread and further mutations.
- It was hard enough to get people to wear masks
It took months to get to the point where masks became the standard, so breaking that standard will send a very mixed message to others and may discourage people with mask-fatigue from wearing them.
- The vaccine doesn’t guarantee 100% immunity…
…But it’s close, and that’s why I put this reason last. The mRNA vaccines (Pfizer/BioNTech and Moderna) provide around 95% immunity, and the other vaccines have varying ranges (Novavax 89%, Johnson and Johnson 72%, and Astra Zeneca 62%). To put this in perspective, the flu vaccine, on a good match year, has around 40-60% effectiveness.
In addition, it takes time to achieve 95% effectiveness. For Pfizer, protection starts 12 days after first shot and reaches 52% effectiveness. After the second shot, it takes 7 days to reach 95% effectiveness. For Moderna, 51% effectiveness is reached 14 days after first shot and 94% effectiveness 14 days after the second shot.
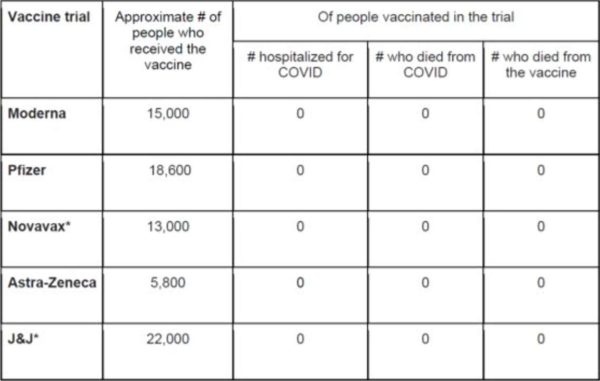
So there is a nonzero chance you can get infected and become severely ill, but it’s a very small chance. Here is a chart that drives that point home. There’s the feel-good story you may be looking for.
Truth be told, even if and when we control COVID, I suspect that masks will become the standard in frontline patient care — much like when glove wearing was implemented during the AIDS epidemic and converted to standard protective gear. Outside the healthcare setting, once the majority of people have been vaccinated and community transmission remain low, then we can start thinking about a mask-free life.
Dr. George C. Hwang, known to his patients as Dr. Chaucer, is a practicing anesthesiologist who also helps to run Mind Peace Clinics in Arlington. He has written for multiple journals, textbooks and medical news outlets, and has been living in Arlington for the past 15 years.