Arlington County is developing an alert system aimed at improving its emergency response to behavioral health crises.
The aim of the system, dubbed the Marcus Alert, is to keep people in crisis — due to a mental illness, substance use disorder or intellectual and developmental disabilities — from being arrested and booked in jail.
It comes from the Marcus-David Peters Act, which was signed into law in late 2020 and is named for Marcus-David Peters, a 24-year-old biology teacher who was killed by a police officer in 2018 while experiencing a mental health crisis.
Once operational, the system would transfer people who call 911 or 988 — a new national suicide and mental health crisis hotline — to a regional call center where staff determine whether to de-escalate the situation over the phone, dispatch a mobile crisis unit or send specially trained law enforcement.
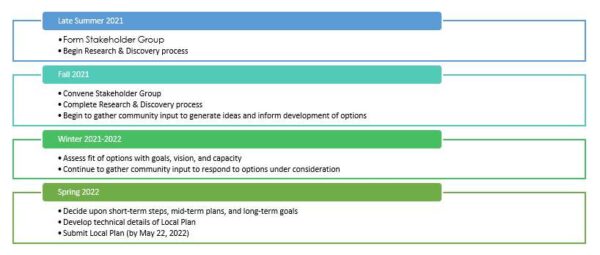
Last summer, Arlington began developing its Marcus Alert plan, a draft of which needs to be submitted to the state by May 22. It’s asking residents to share their experiences with the county’s current behavioral health crisis response via an anonymous and voluntary survey open through mid-March.
Locals can also email the county to sign up to participate in focus groups, which will convene in early- to mid-March.
State law requires that the county’s final plan be implemented by July 1.
“We are hopeful that with the Marcus Alert and increased community outreach and co-response, we will see a reduction in arrests of people with [serious mental illnesses],” Suzanne Somerville, the bureau director of residential and specialized clinical services for Arlington’s Department of Human Services, tells ARLnow. “The system is tremendously strained at this time and hospitalization for people that need it for psychiatric symptoms is not always easy to attain.”
DHS attributes the strain to COVID-19 and a lack of beds in state-run mental hospitals after the Commonwealth closed more than half of these hospitals to new admissions amid its own workforce crisis. This overwhelmed local hospitals and the Arlington County Police Department, and drove fatigued DHS clinicians and Arlington police officers to quit.
“Everyone is trying to do the right thing and get the client the services they need and deserve and we just don’t have the resources currently,” said Aubrey Graham, the behavioral health program manager for the Arlington County jail.
Bed shortages also impact court hearings, as many inmates with mental illnesses require competency restoration services to understand court proceedings and work with their defense attorney. Graham says inmates must go to Virginia Department of Behavioral Health and Developmental Services state hospitals, which limits beds even more.
Compared to other jurisdictions, Arlington sends proportionately more people to Western State Hospital for competency restoration, per data ARLnow requested from DBHDS. It also saw the greatest increase in admission rates between 2020 and 2021.
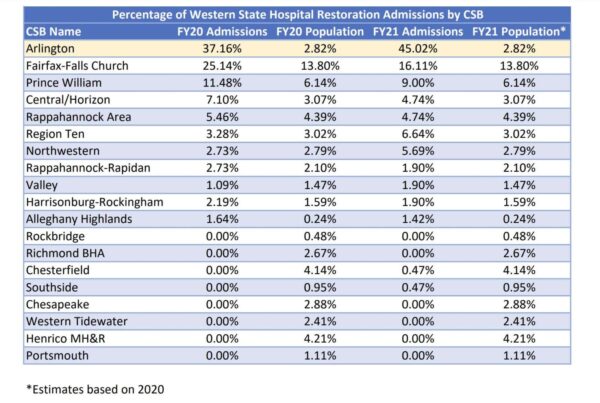
Graham says she doesn’t know of any studies that explain why Arlington sees so many individuals with serious mental illnesses, but geography plays a role, as about 70% of people sent to state hospitals come from D.C., Maryland and other parts of Virginia. Only about 30% of those sent to state hospitals from Arlington are actually Arlington residents.
“Although there are a high number of competency evaluations requested in Arlington courts, the referrals are entirely appropriate, and most are deemed incompetent to stand trial,” Graham said.
That’s why police should not arrest them in the first place, says Chief Public Defender Brad Haywood, adding that people with mental illnesses are over-represented in the county jail, which is seeing a continued inmate deaths and may not have the resources to treat the needs of the mentally ill.